ERP for Healthcare Improving Patient Care and Operations
Introduction to ERP in Healthcare
Enterprise Resource Planning (ERP) systems are transforming healthcare operations by integrating various functions into a single, unified platform. This integration streamlines processes, improves data management, and ultimately enhances patient care and operational efficiency. Unlike disparate systems that often lead to data silos and communication breakdowns, an ERP system provides a holistic view of the organization, facilitating better decision-making and resource allocation.
An ERP system in a healthcare setting centralizes data from various departments, including patient administration, billing and finance, human resources, supply chain management, and clinical operations. Core functionalities include patient registration and scheduling, medical record management, billing and claims processing, inventory management, financial reporting, and human resource management. These functionalities are interconnected, allowing for seamless data flow and reduced manual processes.
Key Benefits of Implementing an ERP System for Healthcare Providers
Implementing an ERP system offers numerous advantages for healthcare providers. These benefits contribute to improved patient care, increased operational efficiency, and enhanced financial performance. Significant improvements can be observed across various aspects of the organization.
- Improved Patient Care: Centralized patient information allows for faster access to medical history, leading to more informed clinical decisions and reduced medical errors. Streamlined appointment scheduling reduces wait times and improves patient satisfaction.
- Enhanced Operational Efficiency: Automation of administrative tasks frees up staff to focus on patient care. Real-time data visibility improves resource allocation and reduces operational costs.
- Increased Revenue Cycle Management Efficiency: Automated billing and claims processing reduces delays in payments and improves cash flow. Real-time financial reporting provides better visibility into revenue and expenses.
- Better Compliance and Risk Management: An ERP system helps healthcare providers maintain compliance with industry regulations and standards, reducing the risk of penalties and legal issues.
- Improved Decision Making: Access to real-time data and comprehensive reporting capabilities enables better informed strategic decision-making.
Types of Healthcare Organizations Benefiting from ERP
The advantages of ERP systems extend across a wide spectrum of healthcare organizations. Various sizes and structures can leverage the benefits of integration and automation.
- Hospitals: Large hospitals can benefit from the comprehensive functionality of an ERP system to manage patient flow, streamline operations, and improve financial performance. For example, a large teaching hospital might use an ERP system to manage its complex billing processes, track research grants, and coordinate multiple departments.
- Clinics and Physician Practices: Smaller clinics and physician practices can utilize ERP systems to manage patient appointments, billing, and inventory, improving efficiency and reducing administrative burden. A small group practice might use an ERP to efficiently manage patient records, streamline scheduling, and automate billing processes, improving patient flow and revenue cycle management.
- Long-Term Care Facilities: Nursing homes and assisted living facilities can use ERP systems to manage resident care, track medication, and manage staffing, ensuring better patient care and regulatory compliance. A large nursing home chain might leverage an ERP to standardize care protocols across multiple locations, improve inventory management of medical supplies, and enhance resident record management.
- Pharmaceutical Companies: ERP systems can aid in managing supply chains, tracking inventory, and ensuring regulatory compliance in pharmaceutical organizations. A large pharmaceutical company could utilize an ERP system to effectively manage its global supply chain, track the production and distribution of medications, and maintain compliance with strict regulatory requirements.
Enhanced Patient Management with ERP

Implementing an Enterprise Resource Planning (ERP) system in a healthcare setting significantly improves patient management by streamlining various processes, reducing administrative burdens, and enhancing the overall patient experience. This leads to improved efficiency, reduced costs, and better patient outcomes. The integrated nature of an ERP system allows for seamless data flow across different departments, creating a holistic view of each patient’s journey.
Improved Patient Registration and Scheduling
ERP systems automate and optimize patient registration and scheduling processes. Instead of manual data entry and paper-based systems, patients can register online or at the point of care through integrated systems. This automation minimizes errors, reduces wait times, and improves the accuracy of patient information. The system can also manage appointment scheduling, send reminders, and handle cancellations efficiently, optimizing resource allocation and minimizing no-shows. For example, an ERP system can automatically check for appointment conflicts, suggest optimal times based on physician availability, and send automated reminders via SMS or email. This ensures that appointment slots are utilized effectively and that patients attend their scheduled appointments.
Management of Patient Medical Records and History
ERP systems provide a centralized repository for all patient medical records and history. This eliminates the need for scattered files and disparate databases, ensuring that all relevant information is readily available to authorized personnel. The system can track patient demographics, medical history, allergies, medications, lab results, and imaging data, providing a comprehensive view of the patient’s health. This facilitates better clinical decision-making, reduces medical errors, and improves the continuity of care. Features such as electronic health records (EHR) integration and secure data storage enhance patient privacy and security. For instance, a physician can quickly access a patient’s complete medical history, including past diagnoses, treatments, and allergies, before a consultation, leading to a more informed and efficient visit.
Enhanced Patient Communication and Engagement
ERP systems enhance patient communication and engagement through various features such as automated appointment reminders, online portals for accessing medical records and test results, and secure messaging systems for communication between patients and healthcare providers. These features improve patient satisfaction and promote better adherence to treatment plans. Patient portals empower patients to actively participate in their care by providing them with convenient access to their health information and facilitating direct communication with their healthcare team. For example, a patient can securely access their lab results online, eliminating the need for phone calls or visits to the clinic.
Hypothetical Scenario: Improved Patient Flow with ERP
Consider a small clinic experiencing long wait times due to inefficient scheduling and manual record-keeping. Implementing an ERP system streamlines patient flow, reducing wait times significantly.
| Before Implementation | After Implementation | Metric | Improvement Percentage |
|---|---|---|---|
| 45 minutes | 15 minutes | Average Wait Time | 66.7% |
| 20% | 5% | No-Show Rate | 75% |
| 10 minutes | 2 minutes | Average Check-in Time | 80% |
| 2 hours | 30 minutes | Average Physician Turnaround Time | 83.3% |
Streamlined Healthcare Operations with ERP
Enterprise Resource Planning (ERP) systems significantly enhance healthcare operational efficiency by integrating various departments and processes onto a single platform. This integration streamlines workflows, reduces redundancies, and improves data visibility, ultimately leading to better patient care and improved financial performance. The benefits extend across multiple areas, including supply chain management, billing and revenue cycle management, and medication management.
Optimized Supply Chain Management in Healthcare
Effective supply chain management is crucial for healthcare providers. ERP systems optimize this by providing real-time visibility into inventory levels, predicting future needs based on historical data and patient demand, and automating ordering processes. This minimizes stockouts of essential supplies, reduces waste from expired or unused items, and ensures timely delivery of necessary medical equipment and pharmaceuticals. For example, an ERP system can track the usage of bandages in a surgical unit, automatically generate an order when stock falls below a predetermined threshold, and schedule delivery to minimize disruptions to surgical procedures. The system can also track the expiry dates of medications, alerting staff well in advance to avoid waste and potential shortages.
Improved Billing and Revenue Cycle Management
ERP systems significantly improve billing and revenue cycle management by automating processes, reducing manual errors, and accelerating payment collection. Features like automated claims submission, real-time eligibility verification, and patient payment tracking streamline the entire revenue cycle. This leads to improved cash flow, reduced administrative costs, and minimized revenue leakage. For instance, an ERP system can automatically generate invoices, send reminders to patients, and track payments, reducing the time spent on manual billing tasks and improving the accuracy of billing information. The system can also integrate with insurance providers to facilitate quicker claim processing and payment reconciliation.
Operational Efficiency Gains: ERP vs. Disparate Systems
Implementing an ERP system offers substantial operational efficiency gains compared to using disparate systems. Disparate systems, where different departments use independent software applications, often lead to data silos, information inconsistencies, and inefficient workflows. This can result in delays, errors, and increased administrative costs. An ERP system, by contrast, integrates all these systems, providing a unified view of the organization’s data and processes. This eliminates redundancies, reduces manual data entry, and improves communication and collaboration across departments. A hospital using a disparate system might experience delays in patient discharge due to difficulties coordinating information between billing, pharmacy, and nursing departments. An ERP system would eliminate these delays by providing a centralized platform for all this information.
Step-by-Step Medication Management Improvement with ERP
- Inventory Management: The ERP system tracks medication inventory levels in real-time, automatically generating purchase orders when stock falls below a predefined threshold. This prevents shortages and ensures timely replenishment.
- Automated Dispensing: Integration with automated dispensing cabinets (ADCs) allows for precise tracking of medication dispensing, reducing medication errors and improving security.
- Clinical Integration: The ERP system integrates with electronic health records (EHRs), providing clinicians with real-time access to patient medication profiles and allergy information, minimizing the risk of adverse drug events.
- Expiration Date Tracking: The system monitors medication expiration dates, alerting staff to potential waste and ensuring the availability of fresh medication.
- Reporting and Analytics: The ERP system provides comprehensive reports on medication usage, costs, and potential waste, enabling data-driven decisions to optimize medication management practices.
Improved Data Management and Analytics
Effective data management is paramount in healthcare, influencing everything from patient care to operational efficiency. ERP systems offer a significant advantage by centralizing and consolidating data from disparate sources across the healthcare organization, creating a unified and readily accessible information repository. This integrated approach fosters better collaboration, reduces data silos, and enables more informed decision-making.
ERP systems achieve data centralization by integrating various departmental systems, such as patient management, billing, inventory, and human resources, into a single platform. This eliminates the need for manual data entry and reconciliation across multiple systems, reducing errors and improving data accuracy. Consolidation involves harmonizing data formats and structures, making it easier to analyze and interpret information across the entire organization. The result is a comprehensive, real-time view of the healthcare organization’s operations and performance.
Data Analytics for Improved Decision-Making
Data analytics within an ERP system transforms raw data into actionable insights, supporting strategic and operational decision-making. Sophisticated analytical tools embedded within ERP platforms allow healthcare providers to identify trends, patterns, and anomalies in patient data, operational performance, and financial metrics. This capability empowers data-driven decision-making, optimizing resource allocation, enhancing operational efficiency, and improving patient outcomes. For example, predictive analytics can forecast patient volumes, enabling proactive staffing adjustments and resource management.
Key Performance Indicators (KPIs) Tracked and Analyzed Using ERP Data
Several key performance indicators can be effectively tracked and analyzed using data housed within an ERP system. These KPIs provide a comprehensive overview of the healthcare organization’s performance across various dimensions. Examples include:
- Average Length of Stay (ALOS): Tracking ALOS helps identify potential areas for improvement in patient care pathways and resource utilization.
- Patient Satisfaction Scores: Analyzing patient feedback data allows for the identification of areas needing improvement in patient experience and service delivery.
- Revenue Cycle Management Metrics: KPIs such as Days in Accounts Receivable (DAR) and claim denial rates provide insights into the efficiency of billing and revenue collection processes.
- Inventory Turnover Rate: This metric helps optimize inventory management, reducing waste and ensuring timely access to essential supplies.
- Staffing Efficiency: Analyzing staff utilization data can highlight areas where staffing levels can be optimized to improve productivity and reduce costs.
Data Security and Privacy Considerations
Implementing an ERP system necessitates a robust approach to data security and privacy to safeguard sensitive patient information. Compliance with regulations such as HIPAA (in the US) and GDPR (in Europe) is crucial. Key considerations include:
- Access Control: Implementing role-based access control to restrict access to sensitive data based on individual roles and responsibilities.
- Data Encryption: Encrypting data both in transit and at rest to protect against unauthorized access.
- Regular Security Audits: Conducting regular security audits and vulnerability assessments to identify and address potential security weaknesses.
- Employee Training: Providing employees with training on data security best practices and awareness of potential threats.
- Data Backup and Disaster Recovery: Implementing robust data backup and disaster recovery plans to ensure business continuity in the event of a system failure or security breach.
Enhanced Staff Collaboration and Communication
Effective communication and collaboration are paramount in healthcare, directly impacting patient safety and the overall efficiency of operations. An Enterprise Resource Planning (ERP) system significantly enhances these crucial aspects by providing a centralized platform for information sharing and task management among diverse healthcare teams. This integrated approach streamlines workflows, reduces errors, and improves the overall quality of care.
ERP systems facilitate better communication and collaboration by centralizing information. Instead of relying on disparate systems and methods of communication, such as emails, phone calls, and paper-based records, healthcare staff can access a single, unified source of patient data, schedules, and communication tools. This eliminates information silos and ensures everyone is working with the most up-to-date information. For instance, a nurse can instantly access a patient’s complete medical history, including allergies and medication details, from the ERP system, facilitating more informed care decisions and reducing the risk of medication errors. Doctors can also update patient records in real-time, ensuring that all members of the care team have access to the latest information.
Staff Scheduling and Assignment Management
ERP systems provide robust tools for managing staff schedules and assignments. These tools optimize staffing levels based on patient demand, skill sets, and availability, minimizing labor costs while ensuring adequate coverage. Features such as automated scheduling, shift swapping capabilities, and real-time tracking of staff attendance improve efficiency and reduce administrative burden. For example, an ERP system can automatically generate staff schedules based on pre-defined rules and constraints, such as ensuring sufficient nurses are on duty during peak hours or assigning specialists to specific procedures. The system can also track staff attendance and automatically generate reports on overtime hours, aiding in payroll processing and workforce management. This automated approach reduces the administrative workload associated with manual scheduling and minimizes scheduling conflicts.
Staff Training and Development
ERP systems can play a crucial role in improving staff training and development by providing a platform for managing training programs, tracking employee competencies, and facilitating knowledge sharing. The system can be used to assign training modules to employees based on their roles and skill gaps, track their progress, and generate reports on training completion rates. This ensures that staff receive the necessary training to perform their jobs effectively and maintain their skills up-to-date. For example, an ERP system can automatically assign mandatory compliance training modules to all employees, ensuring that everyone meets regulatory requirements. The system can also track the completion of training modules and generate reports on employee competencies, which can be used to identify training needs and improve the overall quality of care. This ensures continuous professional development, improving both individual and organizational performance.
Cost Savings and ROI from ERP Implementation
Implementing an Enterprise Resource Planning (ERP) system in a healthcare setting offers significant opportunities for cost reduction and a strong return on investment (ROI). While the initial investment can be substantial, the long-term benefits often outweigh the upfront costs, leading to improved efficiency, reduced operational expenses, and enhanced revenue generation. This section will detail the potential cost savings and factors influencing the ROI of an ERP system in healthcare.
The potential cost savings associated with implementing an ERP system are multifaceted. By automating processes, reducing manual data entry, and streamlining workflows, healthcare providers can significantly reduce labor costs. Improved inventory management, facilitated by ERP systems, minimizes waste and reduces storage costs. Furthermore, optimized scheduling and resource allocation contribute to increased operational efficiency and decreased expenses. Enhanced data analytics capabilities allow for better decision-making, leading to more effective resource utilization and cost avoidance.
Cost Reduction through Process Automation
ERP systems automate many time-consuming manual tasks, such as billing, scheduling, and inventory management. This automation frees up staff to focus on patient care and other high-value activities. For example, automating appointment scheduling can reduce no-show rates, leading to improved resource utilization and reduced revenue loss. Similarly, automating billing processes can speed up payments and reduce the time spent on manual reconciliation, resulting in substantial cost savings. A study by a leading healthcare consulting firm found that automation of administrative tasks through ERP implementation resulted in a 15-20% reduction in administrative staff hours within a year in a medium-sized hospital.
Factors Influencing Return on Investment (ROI)
Several factors influence the ROI of an ERP system. These include the initial investment cost, implementation time, the system’s functionality and scalability, the level of staff training required, and the ongoing maintenance costs. The size and complexity of the healthcare organization also play a significant role. Larger organizations with more complex operations may see a higher ROI, while smaller organizations may experience quicker returns on their investment. Effective project management and change management are crucial for ensuring a successful implementation and maximizing ROI. Accurate forecasting of cost savings and revenue increases is also essential for a realistic ROI projection.
Tangible and Intangible Benefits Contributing to ROI
The ROI of an ERP system encompasses both tangible and intangible benefits. Tangible benefits include measurable cost savings, such as reduced labor costs, improved inventory management, and decreased administrative expenses. These can be quantified and included in a financial model to demonstrate the return on investment. Intangible benefits, while harder to quantify, are equally important. These include improved patient satisfaction, enhanced staff morale, better decision-making, and improved compliance with regulatory requirements. For instance, improved patient satisfaction can lead to increased patient loyalty and referrals, contributing to revenue growth. Similarly, enhanced staff morale can lead to reduced staff turnover, resulting in cost savings associated with recruitment and training. A well-implemented ERP system can contribute to better patient outcomes, a crucial intangible benefit that indirectly impacts the bottom line through reduced readmissions and improved overall health.
Integration with Other Healthcare Systems
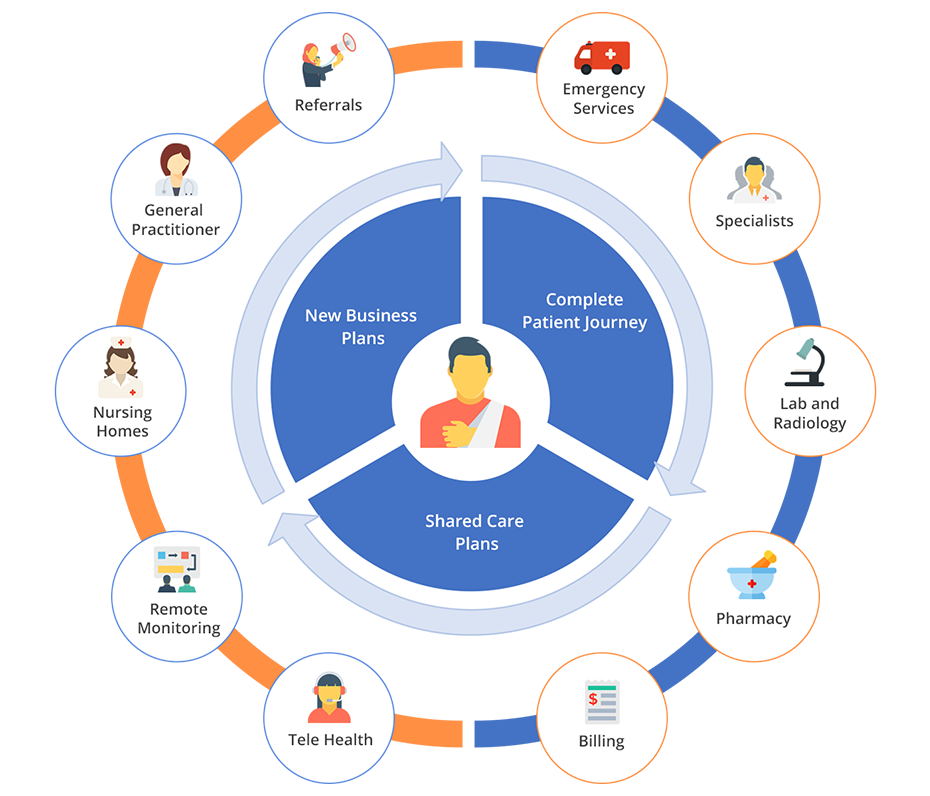
Effective ERP implementation in healthcare requires seamless integration with existing systems to avoid data silos and maximize operational efficiency. A well-integrated ERP system acts as a central hub, connecting disparate data sources and streamlining workflows across the entire organization. This integration is crucial for achieving the full potential of an ERP system in improving patient care and operational outcomes.
ERP systems integrate with electronic health records (EHR) and other healthcare IT systems through various methods, including application programming interfaces (APIs), data exchange standards like HL7, and middleware solutions. APIs allow different systems to communicate and exchange data in real-time, while HL7 provides a standardized format for exchanging clinical data. Middleware acts as a translator, facilitating communication between systems with different architectures and protocols. This interconnectedness allows for a holistic view of patient data, improving decision-making and reducing the risk of errors.
Methods of System Integration
Successful integration involves careful planning and execution. The chosen method depends on the specific systems involved, their technical capabilities, and the organization’s overall IT infrastructure. A phased approach, starting with high-priority integrations, is often recommended to minimize disruption and ensure a smooth transition. Robust data validation and security measures are also essential to maintain data integrity and patient privacy.
Challenges and Considerations in System Integration
Several challenges can arise during the integration process. These include data compatibility issues, differing data structures and formats across systems, the need for extensive data mapping and transformation, and the potential for integration-related downtime. Furthermore, ensuring data security and compliance with regulations like HIPAA is paramount. Careful consideration should be given to the selection of integration technologies and the development of comprehensive integration plans. A skilled IT team with expertise in healthcare systems integration is crucial for successful implementation.
Examples of Successful ERP Integrations
Several healthcare organizations have successfully integrated ERP systems with their existing IT infrastructure. For example, a large hospital system might integrate its ERP system with its EHR to streamline billing and revenue cycle management, improving efficiency and reducing administrative costs. Another example could be a clinic integrating its ERP with a patient portal to enhance communication and patient engagement, allowing patients to access their medical records and schedule appointments online. These successful integrations demonstrate the potential for improved patient care, operational efficiency, and cost savings when ERP systems are properly integrated with other healthcare IT systems. The key to success lies in careful planning, robust testing, and ongoing maintenance of the integrated systems.
Security and Compliance in Healthcare ERP: ERP For Healthcare: How It Improves Patient Management And Operations
Implementing an ERP system in a healthcare setting necessitates robust security measures and strict adherence to relevant regulations to safeguard sensitive patient data. Failure to do so can lead to significant legal and reputational damage, not to mention the ethical implications of compromising patient privacy. This section details the critical security and compliance considerations for healthcare ERP systems.
ERP for Healthcare: How It Improves Patient Management and Operations – Effective security and compliance are paramount for maintaining patient trust and ensuring the long-term success of an ERP implementation. A multi-layered approach, encompassing technological safeguards, procedural protocols, and staff training, is crucial for mitigating risks and adhering to regulatory standards.
Data Encryption and Access Control
Data encryption, both in transit and at rest, is a fundamental security measure. This involves converting sensitive data into an unreadable format, protecting it from unauthorized access even if a breach occurs. Access control mechanisms, such as role-based access control (RBAC), ensure that only authorized personnel can access specific data based on their job responsibilities. For example, a billing clerk might have access to financial data but not to patient medical records. Multi-factor authentication (MFA), requiring multiple forms of verification (e.g., password and a one-time code), adds an extra layer of security to user logins.
HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) in the United States sets stringent standards for protecting the privacy and security of Protected Health Information (PHI). Compliance with HIPAA requires implementing administrative, physical, and technical safeguards to protect PHI. This includes developing and implementing comprehensive policies and procedures for data security, conducting regular security risk assessments, and providing employee training on HIPAA regulations. Penalties for non-compliance can be substantial, including significant fines and legal action. Organizations must maintain a detailed audit trail of all access to PHI, facilitating investigations and demonstrating compliance.
Data Backup and Disaster Recovery
Robust data backup and disaster recovery (DR) plans are essential for ensuring business continuity and data protection in the event of unforeseen circumstances, such as natural disasters, cyberattacks, or system failures. Regular backups should be performed and stored securely, ideally in a geographically separate location. A comprehensive DR plan should Artikel procedures for restoring data and systems in a timely manner, minimizing disruption to operations. This plan should include testing and validation to ensure its effectiveness. For instance, a hospital might utilize cloud-based backup solutions and a secondary data center to ensure rapid recovery in case of a primary site failure.
Choosing the Right ERP System for Healthcare
Selecting the appropriate Enterprise Resource Planning (ERP) system is crucial for healthcare organizations seeking to optimize operations, improve patient care, and enhance financial performance. A poorly chosen system can lead to integration challenges, workflow disruptions, and ultimately, hinder the very benefits an ERP is intended to provide. Careful consideration of several key factors is essential to ensure a successful implementation.
Key Factors in ERP System Selection
The selection process requires a thorough evaluation of various aspects. These range from the system’s functionality and scalability to its vendor’s reputation and support capabilities. Ignoring any of these could lead to significant problems down the line. A robust evaluation process minimizes risks and maximizes the chances of a successful ERP implementation.
- Organizational Needs and Goals: Clearly define the organization’s specific requirements and objectives for the ERP system. This includes identifying key pain points, desired improvements in processes, and long-term strategic goals. For example, a hospital focusing on patient experience might prioritize features related to patient portal integration and appointment scheduling, while a clinic focused on billing might prioritize features related to claims processing and revenue cycle management.
- System Functionality and Features: The chosen ERP must seamlessly integrate with existing systems and provide the necessary functionalities to support core healthcare processes, such as patient management, billing, scheduling, and supply chain management. Consider the specific modules required (e.g., electronic health record (EHR) integration, pharmacy management, laboratory information systems (LIS)).
- Scalability and Flexibility: The system should be scalable to accommodate future growth and adaptable to changing organizational needs. A system that cannot handle increased patient volume or new functionalities will quickly become a bottleneck.
- Vendor Reputation and Support: Thoroughly research potential vendors, assessing their experience in the healthcare industry, track record of successful implementations, and the level of ongoing support they provide. Customer references and case studies can provide valuable insights.
- Cost and Return on Investment (ROI): Evaluate the total cost of ownership, including implementation costs, licensing fees, maintenance, and training. Develop a clear ROI model to justify the investment and demonstrate the long-term benefits of the ERP system.
- Integration Capabilities: The ERP system must seamlessly integrate with existing healthcare information systems, such as EHRs, practice management systems, and billing systems. This ensures data consistency and minimizes data entry duplication.
Types of ERP Systems for Healthcare, ERP for Healthcare: How It Improves Patient Management and Operations
Different ERP systems cater to the varying needs of healthcare organizations, ranging from small clinics to large hospital systems. Understanding these differences is vital for making an informed decision. The choice depends heavily on the size and complexity of the healthcare organization.
- Cloud-based ERP: Offers accessibility, scalability, and reduced IT infrastructure costs. Examples include systems from Epic and Cerner that offer cloud-based options alongside on-premise solutions. This option is particularly attractive for smaller organizations with limited IT resources.
- On-premise ERP: Provides greater control over data security and customization but requires significant IT infrastructure investment and ongoing maintenance. This approach is often favored by larger healthcare organizations with dedicated IT departments and specific security requirements.
- Hybrid ERP: Combines aspects of cloud-based and on-premise systems, allowing organizations to leverage the benefits of both approaches. For instance, a hospital might host sensitive patient data on-premise while using cloud-based modules for less critical functions.
Essential Features of a Healthcare ERP System
A comprehensive checklist of essential features ensures the selected system adequately addresses the organization’s needs. Prioritizing these features streamlines the selection process and minimizes the risk of overlooking crucial functionalities.
- Patient Management: Comprehensive patient data management, including demographics, medical history, appointments, and insurance information.
- Financial Management: Streamlined billing and claims processing, revenue cycle management, and financial reporting.
- Supply Chain Management: Inventory management, procurement, and distribution of medical supplies and equipment.
- Human Resources Management: Employee management, payroll processing, and time and attendance tracking.
- Reporting and Analytics: Real-time dashboards and reporting tools for monitoring key performance indicators (KPIs) and making data-driven decisions.
- Security and Compliance: Robust security features to protect sensitive patient data and ensure compliance with HIPAA and other relevant regulations.
- Integration with EHR: Seamless integration with existing or planned electronic health record (EHR) systems.
Future Trends in Healthcare ERP
The healthcare landscape is constantly evolving, driven by technological advancements and shifting patient expectations. These changes necessitate the continuous adaptation of Enterprise Resource Planning (ERP) systems to maintain efficiency, improve patient care, and enhance overall operational effectiveness. Future healthcare ERP systems will be characterized by increased intelligence, seamless integration, and a heightened focus on security and compliance.
The integration of cutting-edge technologies is reshaping the capabilities and functionality of healthcare ERP systems. This evolution is driven by the need for improved data analysis, enhanced decision-making, and more personalized patient experiences. The adoption of these technologies promises to streamline workflows, reduce operational costs, and ultimately lead to better patient outcomes.
Artificial Intelligence and Machine Learning in Healthcare ERP
Artificial intelligence (AI) and machine learning (ML) are poised to revolutionize healthcare ERP systems. AI-powered predictive analytics can forecast patient needs, optimize resource allocation, and improve operational efficiency. For example, an AI algorithm integrated into an ERP system could predict potential hospital readmissions based on patient data, allowing proactive interventions to improve patient outcomes and reduce costs. ML algorithms can also automate tasks such as appointment scheduling, billing, and claims processing, freeing up staff to focus on more critical aspects of patient care. The use of these technologies allows for more accurate forecasting of staffing needs, better inventory management, and more efficient allocation of resources, ultimately leading to cost savings and improved service delivery.
Cloud Computing and Mobile Accessibility in Healthcare ERP
Cloud computing offers significant advantages for healthcare ERP systems, including scalability, cost-effectiveness, and enhanced accessibility. A cloud-based ERP system allows healthcare providers to access data and applications from anywhere, anytime, using various devices. This is particularly beneficial for remote healthcare settings or situations requiring immediate access to patient information. Mobile accessibility empowers healthcare professionals with real-time access to critical patient data, enabling quicker and more informed decision-making at the point of care. For instance, a physician using a mobile device can access a patient’s complete medical history, lab results, and medication list directly from the cloud-based ERP system, ensuring continuity of care and improving the overall patient experience. This enhanced accessibility also facilitates better collaboration among healthcare providers, regardless of their physical location.
Query Resolution
What are the common challenges faced during ERP implementation in healthcare?
Common challenges include data migration complexities, integration with existing systems, staff training and adoption, and ensuring compliance with regulations like HIPAA.
How long does it typically take to implement a healthcare ERP system?
Implementation timelines vary depending on the size and complexity of the organization and the chosen ERP system. It can range from several months to over a year.
What is the average cost of implementing a healthcare ERP system?
The cost varies greatly based on factors like system size, customization needs, and implementation services. It’s essential to obtain detailed quotes from vendors.
How does ERP improve staff satisfaction?
ERP streamlines workflows, reduces administrative burden, and improves communication, leading to increased staff efficiency and job satisfaction.